Periodontitis, CRP & IL-6 — How Gum Disease Drives Systemic Inflammation
Luthra S. Treatment of periodontitis and C-reactive protein — J Clin Periodontol (2023). PMID: 35946825. PubMed Link: https://pubmed.ncbi.nlm.nih.gov/35946825/
Machado V. Serum C-Reactive Protein and Periodontitis: A Systematic Review — Frontiers in Immunology (2021). PMID: 34394107. PubMed Link: https://pubmed.ncbi.nlm.nih.gov/34394107/
The Oral Microbiome and Systemic Inflammation: Why Your Gums Raise Your CRP & IL-6
Chronic periodontal disease is not just a local problem. It raises systemic inflammatory markers — notably interleukin-6 (IL-6) and C-reactive protein (CRP) — that are directly implicated in cardiovascular disease, diabetes progression, and other chronic conditions. Treating periodontitis reduces these markers by an amount comparable to standard lifestyle interventions, making oral health a potent lever for lowering systemic inflammation.
Identify pathogens linked to systemic inflammation and act early.
Order Your Perio Protect Kit Now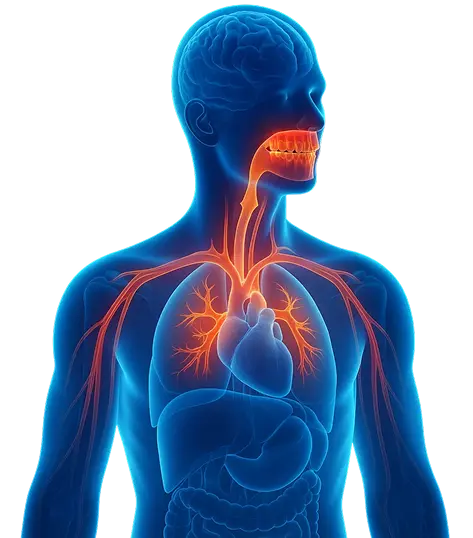
ABOUT THE EVIDENCE
Summary
Multiple high-quality systematic reviews and randomized trials show that periodontitis is associated with
higher serum levels of CRP and IL-6, and that periodontal therapy (especially non-surgical periodontal treatment, NSPT)
reduces these markers in the short–to–medium term. The magnitude of CRP reduction after treatment is clinically meaningful
and supports a causal role of periodontal inflammation in systemic inflammatory burden.
Key Findings
- Elevated inflammatory markers: People with moderate-to-severe periodontitis have higher circulating CRP and IL-6 levels compared with matched healthy controls.
- CRP reduction after treatment: Meta-analyses of randomized clinical trials show that periodontal therapy reduces serum CRP, with average reductions of approximately ~0.6–0.8 mg/L at 3–6 months in pooled estimates.
- IL-6 response to therapy: Non-surgical periodontal therapy (NSPT) and intensive periodontal interventions also significantly reduce IL-6 levels across multiple trials and systematic reviews.
- Comparable to lifestyle effects: The reduction in inflammatory markers following periodontal therapy is comparable to effects observed with lifestyle interventions such as weight loss and smoking cessation in some analyses—indicating strong clinical relevance.
- Cardiometabolic implications: Lowering systemic inflammation through oral treatment may reduce downstream cardiometabolic risk; however, large long-term randomized trials powered for hard cardiovascular outcomes are still limited.
Mechanism (Mouth → Cytokines → Organ Risk)
How periodontal inflammation raises CRP & IL-6
- Local infection: Periodontal pockets harbor gram-negative bacteria and produce local cytokines such as IL-1β, IL-6, and TNF-α.
- Cytokine spillover / bacteremia: Periodontal inflammation permits translocation of bacterial products (LPS) and cytokines into the bloodstream during routine daily activities.
- Hepatic acute-phase response: IL-6 stimulates the liver to synthesize CRP and other acute-phase proteins, increasing circulating CRP. Elevated CRP reflects systemic low-grade inflammation linked to atherosclerosis and insulin resistance.
- Sustained risk: Chronic elevation of CRP and IL-6 promotes endothelial dysfunction, plaque progression, and long-term metabolic dysregulation.
CLINICAL RELEVANCE
Why Patients & Clinicians Should Care
- Validated risk markers: CRP and IL-6 are established prognostic biomarkers — higher levels predict cardiovascular events and poorer metabolic control. If periodontitis elevates these markers, it becomes a modifiable contributor to systemic disease.
- Actionable treatment effect: Treating periodontitis reduces systemic inflammation. Meta-analytic evidence shows consistent reductions in CRP (and frequently IL-6) after periodontal therapy — an objective outcome that can be measured and used to motivate patients.
- Clinical use case for Dentulu: Salivary pathogen testing can identify high-risk profiles (high pathogen load) and direct earlier intervention. After treatment, serial CRP/hs-CRP monitoring (or repeat salivary testing) can demonstrate measurable improvement — a strong conversion driver from test → consult → treatment.
Lower Your Inflammatory Burden — Start with a Saliva Test
Learn whether pathogenic oral bacteria are elevating your CRP/IL-6 risk profile.
Order Your Perio Protect Kit NowRELATED RESEARCH
- Periodontal Disease & Cardiometabolic Risk
- Periodontal Treatment and Biomarker Changes (NSPT Outcomes)
- Salivary Biomarkers vs Serum Biomarkers: Concordance and Clinical Uses
- Diabetes & Oral Inflammation
Have questions? Get answers
References
- Luthra S, et al. (2023): Treatment of periodontitis and C-reactive protein: A systematic review and meta-analysis of randomized clinical trials. Journal of Clinical Periodontology. PMID: 35946825. View on PubMed
- Machado V, et al. (2021): Serum C-Reactive Protein and Periodontitis: A Systematic Review. Frontiers in Immunology. PMID: 34394107. Read Full Article
- Gani DK, et al. (2009): Evaluation of C-reactive protein and interleukin-6 in periodontal disease. PMC Open Access Article. View on PMC
- Meng R, et al. (2024): Effect of non-surgical periodontal therapy on serum CRP and IL-6: Systematic review & meta-analysis. View Meta-Analysis
- Vachhani KS, et al. (2021): Non-surgical periodontal therapy decreased hs-CRP in chronic kidney disease patients — supporting clinical trial evidence. View Study