Oral Microbiome & Metabolic Syndrome: Can Mouth Bacteria Predict Obesity and Metabolic Risk?
Representative primary / review citations:
Si J et al., Oral Microbiota: Microbial Biomarkers of Metabolic Syndrome (2017).
PubMed: https://pubmed.ncbi.nlm.nih.gov/29326886/
Prince Y et al., The Relationship between the Oral Microbiota and Metabolic Syndrome (2022).
PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC9855685/
Schamarek I et al., The role of the oral microbiome in obesity and metabolic disease (2023).
PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC10223863/
The Oral Microbiome and Metabolic Health: Could Your Saliva Predict Diabetes, Obesity, and Metabolic Syndrome?
Metabolic syndrome — the cluster of high blood pressure, central obesity, dyslipidemia, and insulin resistance — fuels the global rise in diabetes and heart disease. Recent research shows that oral microbiome patterns (specific bacterial signatures and dysbiosis) are consistently different in people with obesity and metabolic syndrome, and may even predict metabolic risk before clinical disease appears.
Take control of your oral health now!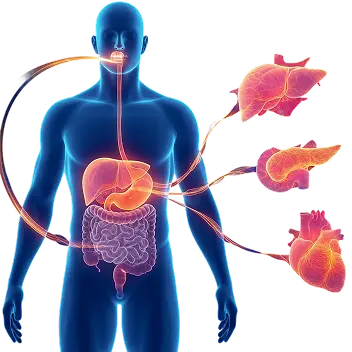
About the Study / Evidence Base
Summary
Multiple case–control and cohort studies, plus mechanistic animal work and human metabolic profiling, show that the oral microbiome differs in people with metabolic syndrome, obesity, and insulin resistance. Specific taxa (for example, Granulicatella, Neisseria, Porphyromonas) and reduced diversity are repeatedly associated with adverse metabolic traits. Evidence supports several plausible routes (oral→gut seeding, systemic inflammation, metabolite signaling) by which oral microbes could contribute to metabolic dysregulation.
Key Findings
- Oral dysbiosis is associated with MetS and obesity: Multiple human studies find distinct oral microbiome signatures in people with metabolic syndrome or obesity versus healthy controls.
- Specific taxa linked to MetS: Studies report enrichment of species such as Granulicatella and Neisseria in MetS, and depletion of taxa like Peptococcus in healthy controls in some cohorts.
- Oral → gut axis and metabolites: Oral microbes can be swallowed or translocate to the gut, altering gut composition and generating metabolites (e.g., LPS, short-chain fatty acids, BCAAs) that affect insulin sensitivity and inflammation.
- Predictive potential: Machine-learning models trained on oral microbiome features can modestly predict metabolic traits (waist circumference, fasting glucose, triglycerides) in cohort studies — indicating potential as a noninvasive risk-screening tool.
- Intervention plausibility: Animal models and small human intervention studies suggest altering oral microbiota (improved oral hygiene, periodontal treatment, targeted antimicrobials) can reduce systemic inflammation and improve metabolic markers — though large trials are limited.
Mechanism (Mouth → Gut/Systemic → Metabolic Dysfunction)
How oral microbes may contribute to metabolic syndrome
- Oral dysbiosis & periodontal inflammation: Chronic periodontal disease increases local inflammation and bacterial load.
- Microbial translocation to the gut: Swallowed oral bacteria can alter gut ecology (oral–gut axis), promoting dysbiosis that favors metabolic endotoxemia.
- Metabolic signaling & inflammation: Oral-derived bacterial products (LPS, proteases) and microbial metabolites (e.g., branched-chain fatty acids) can provoke systemic inflammation, insulin resistance, and adipose dysfunction.
- Host response: The chronic low-grade inflammation (IL-6, CRP) driven by these processes contributes to hypertension, dyslipidemia, and glucose dysregulation seen in metabolic syndrome.
This pathway is biologically plausible and supported by a mixture of observational human data, mechanistic animal work and metabolomic studies.
Clinical Relevance
Why patients should care
- Metabolic syndrome is common and often silent — early detection of risk via a noninvasive salivary test could create a prevention window.
- Oral health is modifiable — improving periodontal status and reducing oral pathogen load may lower systemic inflammation and metabolic risk markers.
- Actionable clinical use case for Dentulu: Salivary microbiome profiling can be used as a screening tool in primary care, wellness programs, or weight-management clinics to prioritize preventive care (dental referral, lifestyle interventions).
- Not a single-cause story: Oral microbes are one of several interacting drivers (diet, genetics, gut microbiome); but they are accessible and modifiable — an attractive target for early intervention.
Screen Your Oral Microbiome for Metabolic Risk
Noninvasive saliva testing can reveal high-risk oral microbial profiles associated with obesity and MetS.
Take control of your oral health now!Related Research
- Periodontitis & Insulin Resistance
- Salivary Biomarkers for Diabetes Risk
- Oral–Gut Axis and Cardiometabolic Health
- Obesity, Microbiome, and Systemic Inflammation
Have questions? Get answers
References
-
Si J, et al. Oral Microbiota: Microbial Biomarkers of Metabolic Syndrome. Scientific Reports / related review. 2017.
PMID: 29326886.
https://pubmed.ncbi.nlm.nih.gov/29326886/ -
Prince Y, et al. The Relationship between the Oral Microbiota and Metabolic Syndrome. Translational Research / review. 2022.
PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC9855685/ -
Schamarek I, et al. The role of the oral microbiome in obesity and metabolic disease. 2023.
PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC10223863/